Keratoconus is a condition in which the cornea, the window of the eye, becomes thin and cone-shaped. The cornea is a very important part of our eye. Light enters and the clear cornea plays a large role in focusing, also called refracting, the light so we can see a clear image. Keratoconus changes the shape of the cornea, which can distort the way the light enters and therefore distorts vision.
What Causes Keratoconus?
We are still not sure what causes Keratoconus, but some research suggests that it could be genetic. Approximately 13% of people with Keratoconus will also have a family member with the condition.
Eye rubbing, eye diseases (retinitis pigmentosa, retinopathy of prematurity, vernal keratoconjunctivitis), and systemic diseases (Down syndrome, osteogenesis imperfect, Ehler’s Danlos Syndrome) have all been shown to have an association with keratoconus.
Keratoconus may start in one eye initially, but
Who Gets Keratoconus?
Keratoconus usually begins at puberty and progresses until the patient is in their mid-30s. Each case is different and there is no way to predict how fast or slow it might progress. Males and females are equally affected.
What Are The Symptoms Of Keratoconus?
- Blurry vision
- Distorted vision
- Glare
- Increased light sensitivity
- Frequent glasses prescription changes
- Inability to wear contact lenses
How Is Keratoconus Diagnosed?
- Keratometry: light is focused on the cornea and the reflection is used to determine the curvature of the front surface. Patients with keratoconus will have a much steeper cornea due to the cone shape.
- Corneal Topography: a photograph of the cornea is taken and a topographical map of the corneal surface is produced. This map will show areas of steepening.
- Pachymetry: a device that measures the thickness of the cornea. Patients with keratoconus will have areas of thinning at the cone.
How Is Keratoconus Treated?
- Glasses and soft contact lenses: Acceptable to correct vision during early stages
- Hard Contact Lenses: The smooth surface of the contact lens allows light to enter without being distorted and this helps improve vision
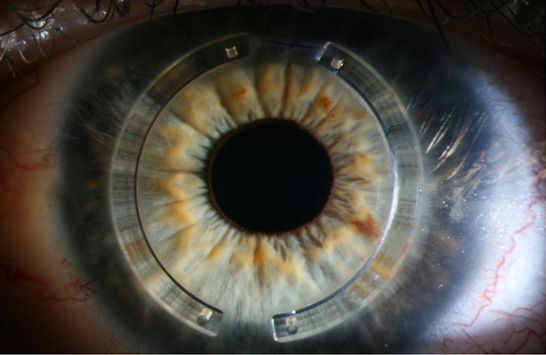
- Intacs: Small curved implants that help flatten the cornea. These must be inserted surgically. Intacs are FDA approved. (See image below).
- Collagen Cross-linking: Vitamin B2 eye drops and UV light are used to help strengthen the cornea. This procedure has been used overseas for years with wonderful results and has just recently been approved by the FDA for use in the United States.
- Corneal Transplant: When good vision is no longer possible or when the cornea has become too thin, corneal transplants are required. The surgeon removes the patient’s cornea and replaces it with a healthy donor cornea. Only about 10-20% of patients with keratoconus require this type of treatment.